Modern life often comes with a steady stream of demands—tight deadlines, endless notifications, and the constant juggling of responsibilities. While a certain level of stress can spark motivation, prolonged strain carries hidden consequences. One of the most profound is its influence on the human immune system, the body’s frontline defense against illness. Understanding the intricate relationship between stress and immunity reveals just how much our mental state shapes physical resilience.

The Connection Between Stress and Immunity
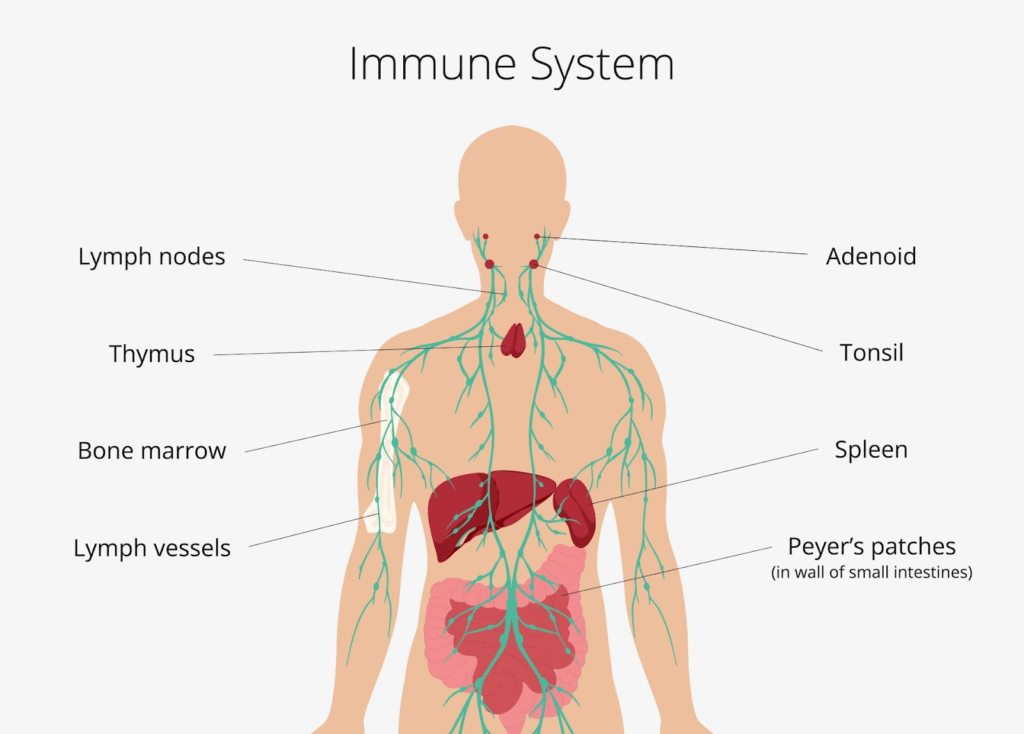
The body is designed to respond swiftly when confronted with challenges. This “fight-or-flight” response, fueled by stress hormones like cortisol and adrenaline, is vital in short bursts. However, when stress lingers, these hormones remain elevated, and the human immune system begins to suffer.
Prolonged human immune stress suppresses the production of white blood cells, weakening the body’s ability to combat viruses, bacteria, and even minor infections. In this state, wounds heal more slowly, colds last longer, and recovery from illness becomes drawn out. Stress essentially diverts resources away from immune defense, prioritizing immediate survival over long-term wellness.
The Subtle Yet Serious Impacts
The human immune impacts of stress extend beyond basic vulnerability to sickness. Chronic stress has been linked to the development and worsening of autoimmune disorders, where the body mistakenly attacks its own tissues. Conditions like rheumatoid arthritis, psoriasis, and inflammatory bowel disease can flare more frequently under persistent strain.
Moreover, stress hampers the body’s ability to produce antibodies after vaccinations. This diminishes protection against diseases that should otherwise be preventable. It’s a silent yet significant consequence of the ongoing tension many individuals carry in their daily lives.
The Biological Mechanisms at Play
At the cellular level, the human immune effects of stress are profound. Elevated cortisol disrupts the balance of cytokines—messenger proteins that regulate inflammation. While some inflammation is necessary for defense, chronic stress tips the balance, causing either excessive or insufficient responses. This imbalance increases the risk of chronic inflammatory conditions and reduces the efficiency of immune cells like natural killer cells and T-cells.
The gut, often called the “second brain,” also plays a central role in immunity. Stress disrupts gut microbiota, the diverse community of bacteria that supports immune regulation. An imbalanced gut environment further weakens the human immune system, leading to digestive problems that compound the body’s vulnerabilities.
Everyday Examples of Stress-Driven Immunity Decline
Consider students preparing for final exams. Research has shown that during exam season, they are more likely to catch colds or suffer from flu-like symptoms. Similarly, caregivers of chronically ill family members often report higher rates of illness themselves. These real-world situations illustrate how human immune stress quietly erodes health over time.
In workplaces, employees experiencing relentless deadlines may notice frequent headaches, recurring colds, or heightened fatigue. These aren’t random coincidences—they are physical signals of the human immune impacts of unrelieved stress.
Building Resilience Through Lifestyle Adjustments
Thankfully, the human immune effects of stress are not irreversible. Lifestyle choices can act as powerful buffers. Regular physical activity, for instance, helps regulate cortisol levels while improving circulation, ensuring immune cells move efficiently throughout the body. Practices like yoga, meditation, and mindful breathing reduce tension and restore balance to the nervous system.
Adequate sleep is equally critical. During deep rest, the body repairs tissues, releases protective cytokines, and fortifies immune memory. By creating a consistent bedtime routine and minimizing late-night screen exposure, individuals can strengthen their natural defenses.
Nutrition also provides a vital shield. Foods rich in antioxidants—berries, leafy greens, and nuts—counteract the oxidative stress caused by prolonged tension. Omega-3 fatty acids from fish or flaxseeds help modulate inflammation, supporting smoother immune responses even under pressure.
The Psychological Dimension of Protection
Equally important is the cultivation of emotional resilience. Social support, laughter, and positive outlooks directly influence the human immune system. Studies suggest that people who feel connected and supported by others show stronger immune responses than those who experience isolation. Stress may be inevitable, but its human immune impacts can be mitigated when individuals have outlets for emotional release and companionship.
The interplay between stress and immunity is undeniable. While short-term stress can sharpen reflexes and enhance alertness, chronic strain gradually undermines the body’s natural defenses. The human immune system is highly sensitive to mental and emotional states, reflecting the deep connection between mind and body.
By addressing human immune stress through mindful practices, balanced nutrition, restorative sleep, and supportive relationships, individuals can protect themselves from the insidious human immune effects of prolonged tension. In doing so, they not only reduce vulnerability to illness but also cultivate a foundation of enduring health and vitality.
More Stories
Human Immune System Wonders Explained
Human Immune Pathways and Your Vitality
Human Immune Support Through Exercise